This is the third article in a series. The first article is here, and the second here.
A week prior to the MSIH graduation in May 2019, students made their final presentations. Before the Directors of MSIH and the Biomedical Engineering Department, the teams explained their projects, thoughts, and ideas, then displayed iterative prototypes – demonstrating how they functioned. Finally, students talked about their experience working together as future physicians and engineers.
Inexpensive yet effective vein locator
First off was the team developing a vein-locating device for intravenous insertion in dehydrated patients.
Insertion of lines is a fundamental part of medical practice, but even in ideal conditions, this can be difficult. Some patients have hard-to-find-veins because of their natural build – other patients may be dehydrated. Some patients are drug addicts making finding a suitable vein difficult. The same if a patient is obese.
Then there’s the skin tone. In light skin, it’s generally easier to locate a vein. It’s harder in dark skin. In very dark skin, it’s harder still – and in very dark skin that’s dehydrated, it’s verging on impossible. For dehydrated dark skin at night, with no lighting, (a midnight drunken car crash, or a patient in an African village) – finding a vein is more a question of luck than competence.
The BGU Vein-Locator Prototype
Commercial devices exist that purport to solve this problem – but they’re designed for modern medical scenarios and may cost hundreds of dollars. What if you’re in an African village with no source of power?
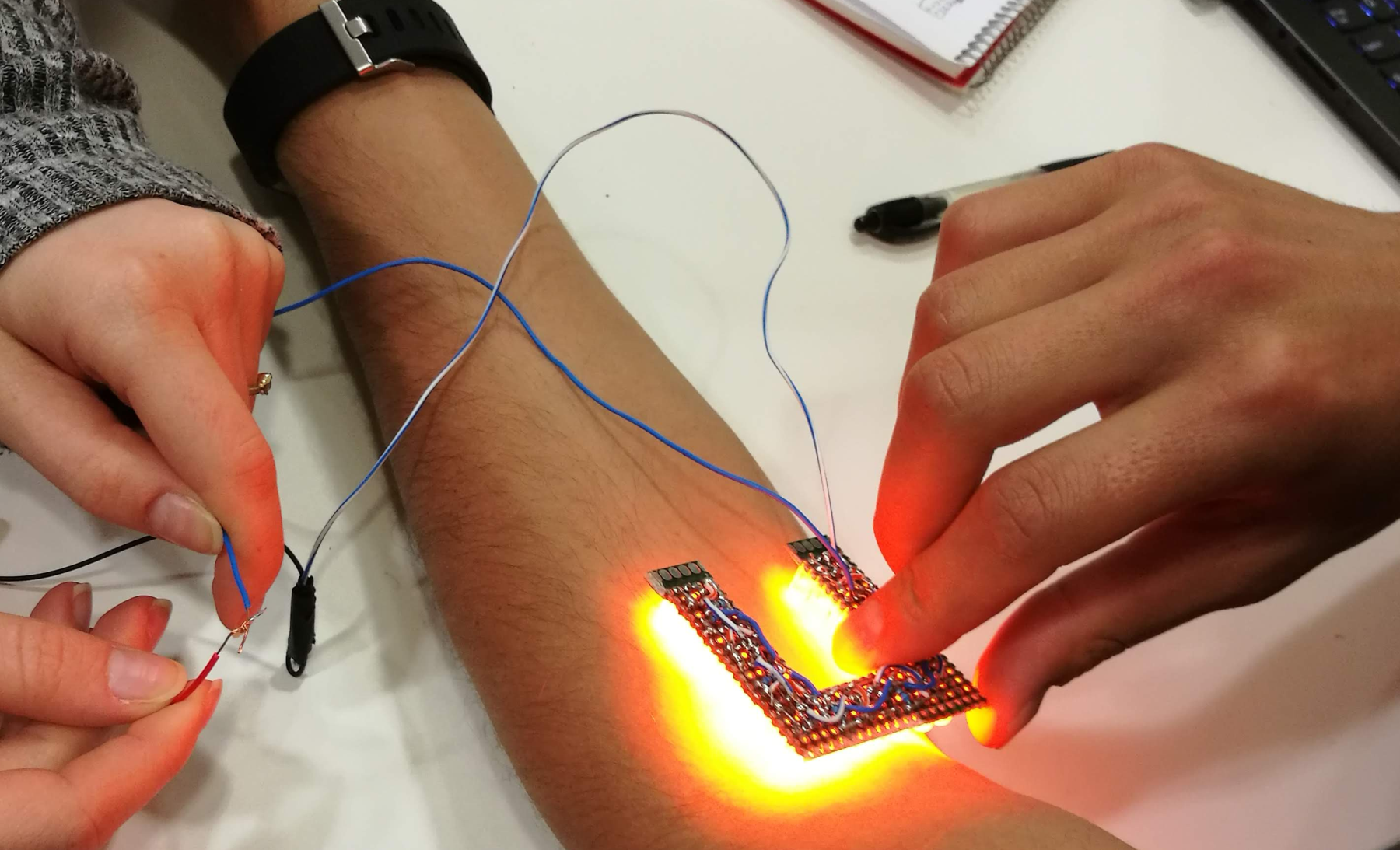
Enter the BGU solution. The head-mounted vein-locator can work off batteries charged by solar panels. Not only is it inexpensive to construct from off-the-shelf LEDs, but it’s portable, resilient and effective – even at night.

Skin Tones
During their trials students began looking into skin tones. They discovered that by changing the frequency of the light (the color of the LED) they could cater to different skins. Theoretically, a single unit could have variable lights to adjust for different skin scenarios.

Another version – that can be strapped around the arm – has a variable resistor that controls light intensity. Note the 3D-printed U-shape case that allows the insertion procedure to be conducted surrounded by light.
Syringe for self-administration of drugs
In low-income countries, patients may live far from the nearest clinic. It’s not unusual for a sick person to walk many miles in harsh terrain to see a doctor. Should the patient need regular injections, he/she will need to make the return journey on foot many times.
Not only is this impractical, but the patient is already weak. Repeatedly walking to the clinic may sap whatever remaining strength there is.
The team wanted to create a syringe for self-administration of drugs. It needed to be easy to use by the patient, safe, inexpensive to produce, non-reusable, and contain just the right dosage for a single injection. It was fundamentally important that once the needle had served its purpose, it would be safely contained – preventing needle-sticking of others and the transmission of disease.

In the above photo, the syringe will contain exactly one dose of the required drug. Once used, the needle collapses inside the container and can’t be accessed again. This is one of several prototypes.
Digital Mapping of Injured Feet – 3D Printing of Personalized Insoles
In low-income countries, diabetes often goes undetected – and untreated. The resultant restricted blood flow can cause severe ulceration of the feet. Large open wounds make it difficult to walk.
In the best-case scenario, a patient may be sent to a specialized shoemaker attached to a hospital. Such shoemakers are few and far between, and even if there is one, lines are long. Patients, unable to walk, can wait for weeks for a pair of cobbled shoes.
A simple camera and 3D printer
With today’s technology, solving this problem is simple. A small computer with attached camera can make a digital map of an injured foot. A bit of processing later and a personalized insole can be sent to a 3D printer using compressible filament. A couple of hours later, the patient can walk out with custom-insoles in regular sandals.

Summing Up
“This was a pilot program,” said Mike Diamond, the innovator behind the project. “This year we brought some enthusiastic students together to see where the project would take us. I was amazed – not only at the quality of the discussions and prototypes – but at the interaction and enthusiasm of students. I won’t forget the comments of one of the BioMed Eng. students. She told me this was the first time they’ve had an opportunity to use their hands and imagination. Until now, all they’d done was mathematics and theory.”
News of the initiative has spread far and wide on the BGU campus and next year promises to see a more organized program.
“Several students have approached me already about getting involved,” said Diamond. “Such is the interest that we’re introducing a module into our Global Health Curriculum – Development of Devices for Low Income Medical Scenarios. I’m confident we’re going to see amazing things.”
The Student Team
This project was run entirely by students of the Department of Biomedical Engineering and MSIH. Special thanks go to Matan Aroosh, Roni Shaashua, and Daniel Levi for their hard work, cooperation, and dedication.